Articular Cartilage is the white tissue lining the end of bones where these bones connect to form joints. Cartilage acts as a cushioning material and forms the smooth articulation of bones during movement. An injury to the joint may damage this cartilage which cannot fully repair on its own. Cartilage can degenerate with increasing age, wear and tear, or trauma. Damaged cartilage cannot cushion the joints during movement and the joints may rub over each other causing pain and inflammation.
Cartilage repair describes surgical procedures where orthopaedic surgeons stimulate the growth of new cartilage that restores more normal function. Degenerate conditions can be delayed or potentially prevented with this type of procedure.
Measures employed for cartilage restoration include dietary supplements, microfracture, drilling, abrasion arthroplasty, osteochondral autograft, and allograft transplantation.
Dietary supplements such as glucosamine and chondroitin are the non-surgical treatment options for cartilage restoration which are used by some patients with good effect. Chrondroitin sulphate and glucosamine are naturally occurring substances that are present within cartilage. Chrondroitin sulphate and glucosamine obtained from animal sources are available as ‘over the counter’ products and are recommended by some for cartilage restoration. Apart from these, various other nutritional supplements are also recommended such as cod liver oil, calcium with magnesium and vitamin D as a combination, S-Adenosyl-Methionine and Methylsulfonylmethane. The evidence for these supplements is mixed.
In this method, numerous holes are created in the injured joint surface using a sharp tool. This procedure stimulates a healing response by creating an injury designed to generate bleeding, healing and a layer of fibrocartilage.
In this method a drilling instrument is used to create holes in the injured joint surface. Drilling holes stimulates a healing response and growth of a new cartilaginous covering. This method is similar to microfracture.
A high speed shaver is used to remove the damaged, unstable cartilage. This procedure is performed using an arthroscope with a ‘key-hole’ procedure.
Healthy cartilage tissue (graft) is taken from an area of the joint that bears less weight and is transferred to the site of cartilage loss. This method is used for smaller cartilage defects. Osteo-articular transfer system (OATS) is a surgical procedure to treat isolated cartilage defects which are limited usually 10 to 20mm in size. The procedure involves transfer of cartilage plugs taken from the non-weight bearing areas of the joint which are then transferred into the damaged areas of the joint. This procedure is not indicated for wide spread damage of cartilage as seen in osteoarthritis.
The procedure is usually performed using ‘key hole surgery’ (arthroscopy). The area of damaged cartilage is prepared using a coring tool which makes a perfectly round hole in the bone in the area of damage. The hole is drilled to a size that fits the harvested plug. Next the plug of normal cartilage/bone is then implanted into the hole that was created in the damaged area. The size of the plug used should be slightly larger than the hole so that it has good ‘press-fit’ in the new location. This procedure allows the newly implanted bone and cartilage to replace the defected area.
Possible complications of OATS include donor site morbidity causing pain, avascular necrosis, and fracture. Other complications such as haemarthrosis, effusion (swelling) and pain may also occur. Following OATS procedures, protected weightbearing rehabilitation is recommended with use of crutches and bracing to limit the range of motion.
A bone/cartilage tissue graft is taken from a human donor and transplanted to the site of the injury. An allograft technique might be recommended if a more significant portion of the joint is damaged.
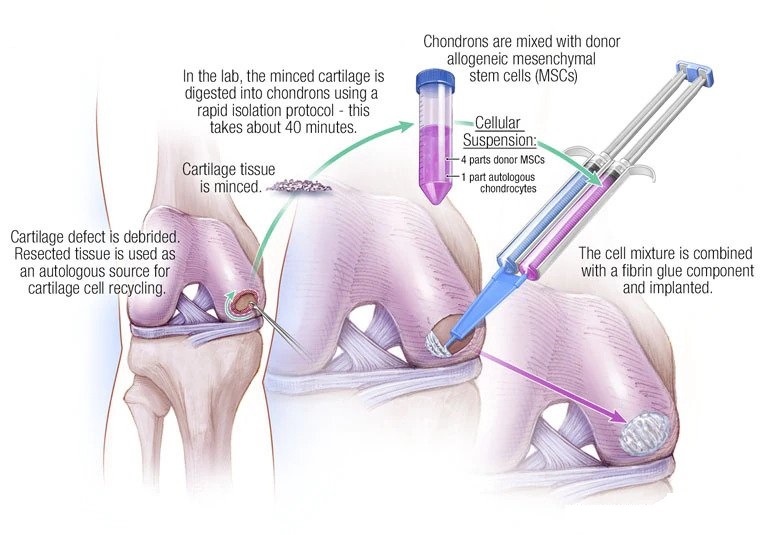
In this method, healthy cartilage cells are removed using an arthroscopic technique and are cultured in a laboratory. Cultured cells can then be implanted in the damaged area with an open surgical technique involving a second surgical procedure.
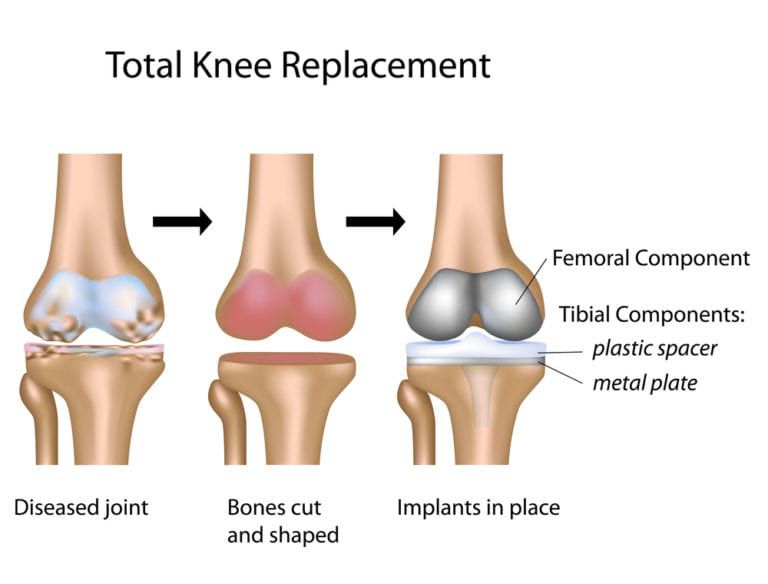
Total knee replacement, also called total knee arthroplasty, is a surgical procedure in which the worn out or damaged surfaces of the knee joint are removed and replaced with an artificial prosthesis.
Total knee replacement, also called total knee arthroplasty, is a surgical procedure in which the worn out or damaged surfaces of the knee joint are removed and replaced with an artificial prosthesis.
Total knee replacement surgery is commonly indicated for severe osteoarthritis of the knee. Osteoarthritis is a type of arthritis. It is the most common form of knee arthritis in which the joint cartilage gradually wears away, and often affects the elderly. Your doctor may advise total knee replacement if you have:
The goal of total knee replacement surgery is to relieve pain and restore the alignment and function of your knee.
Rehabilitation begins immediately following the surgery. A physical therapist will teach you specific exercises to strengthen your leg and restore knee movement. Knee immobilizers are used to stabilize the knee. You will be able to walk with crutches or a walker. A continuous passive motion (CPM) machine can be used to move the knee joint. Continuous passive motion is a device attached to the treated leg that constantly moves the joint through a controlled range of motion, while you are at rest. Your physical therapist will also provide you with a home exercise program to strengthen your thigh and calf muscles.
As with any major surgery, the possible risks and complications associated with total knee replacement surgery include:
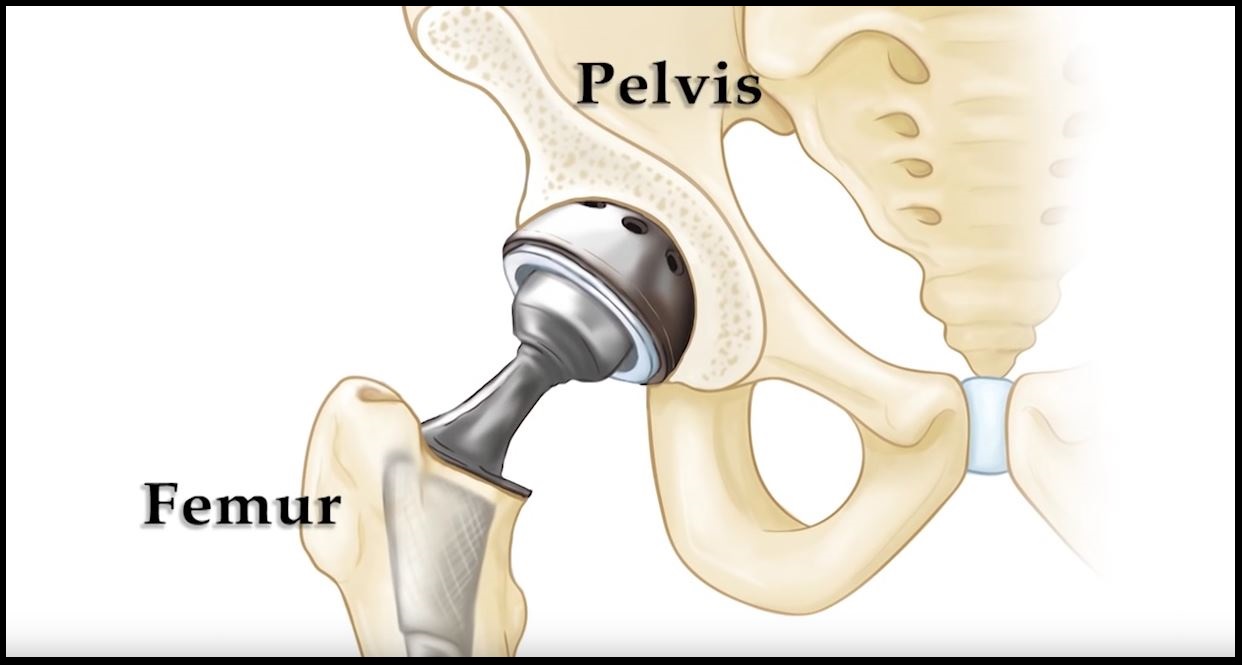
Total hip replacement is a surgical procedure in which the damaged cartilage and bone are removed from the hip joint and replaced with artificial components. The main indication for total hip replacement is arthritis.
Arthritis is the inflammation of joints, which results in pain, swelling, stiffness and limited movement. Hip arthritis is a common cause of chronic hip pain and disability.
The most common symptom of hip arthritis is joint pain and stiffness, resulting in a limited range of motion. Vigorous activity can increase pain and stiffness, which may cause limping while walking.
Diagnosis is made by evaluating your medical history, performing a physical examination and taking X-rays of the arthritic joint.
Surgery may be recommended if conservative treatment options such as anti-inflammatory medications and physical therapy do not relieve your symptoms.
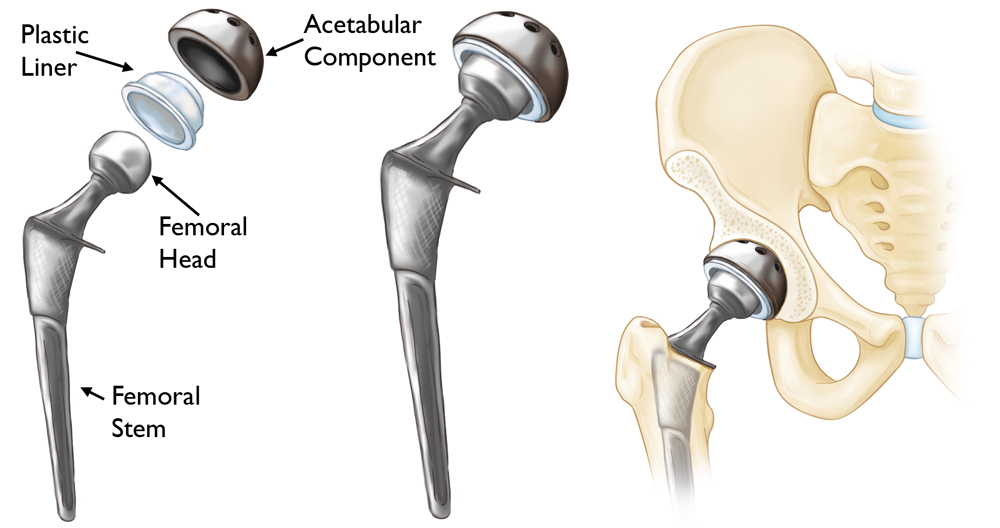
The surgery is performed under general anaesthesia. During the procedure, a surgical cut is made over the hip to expose the hip joint and the femur is dislocated from the acetabulum. The surface of the socket is cleaned and the damaged or arthritic bone removed using a reamer. The acetabular component is inserted into the socket using screws, or occasionally, bone cement. A liner made of plastic, ceramic or metal is placed inside the acetabular component.
The femur or thighbone is then prepared by removing the arthritic bone using special instruments to exactly fit the new metal femoral component. The femoral component is then inserted to the femur either by a press fit or using bone cement. Then the femoral head component made of metal or ceramic is placed on the femoral stem. All the new parts are secured in place using special cement. The muscles and tendons around the new joint are repaired and the incision is closed.
After undergoing total hip replacement, you must take special care to prevent the new joint from dislocating and ensure proper healing. Some of the common precautions to be taken include:
As with any major surgical procedure, there are certain potential risks and complications involved with total hip replacement surgery. The possible complications after total hip replacement may include:
Although total knee replacement surgery is successful, sometimes the procedure can fail due to various reasons and may require revision surgery.
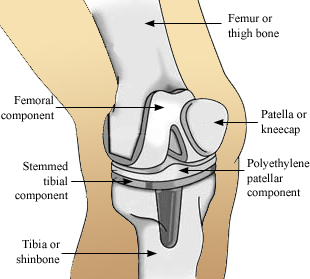
Revision knee replacement surgery involves replacing a part or all your previous knee prosthesis with a new prosthesis. Although total knee replacement surgery is successful, sometimes the procedure can fail due to various reasons and may require a revision surgery.
Revision knee replacement surgery may be advised if you have one or more of the following conditions:
Revision knee replacement surgery may involve the replacement of one or all the components.
The surgery is performed under general anaesthesia. Your surgeon makes an incision over your knee to expose the knee joint. The kneecap along with its ligament may be moved aside so that there is enough room to perform the operation. Then, the old femoral component of the knee prosthesis is removed. The femur is prepared to receive the new component. In some cases, the damaged bone is removed and bone graft or a metal wedge may be used to make up for the lost bone.
Next, the tibial component along with the old plastic liner is removed. The damaged bone is cut and the tibia is prepared to receive the new component. Like the femur, the lost bone is replaced either by a metal wedge or bone graft. Then, a new tibial component is secured to the end of the bone using bone cement. A new plastic liner will be placed on top of the tibial component
If the patella (kneecap) has been damaged, your surgeon will resurface and attach a plastic component. The tibial and femoral components of the prosthesis are then brought together to form the new knee joint, and the knee muscles and tendons are reattached. Surgical drains are placed for the excess blood to drain out and the incision is closed.
Like all major surgical procedures, there may be certain risks and complications involved with revision knee replacement surgery. The possible complications after revision knee replacement include:
Following revision knee replacement surgery, a continuous passive motion (CPM) machine may be used to allow your knee joint to slowly move. The machine, attached to the treated leg, slowly moves the joint through a controlled range of motion, while you are at rest.
You can walk with crutches or a walker. You will be sent for rehabilitation within a couple of days of surgery. A physical therapist will teach you specific exercises to strengthen your leg and restore range of motion to the knee. Your physical therapist will also provide you with a home exercise program to strengthen the thigh and calf muscles.
During total hip replacement, the damaged cartilage and bone are removed from the hip joint and replaced with artificial components. At times, hip replacement implants can wear out for various reasons and may need to be replaced with the help of a surgical procedure known as revision hip replacement surgery.
Revision hip replacement is a complex surgical procedure in which all or part of a previously implanted hip joint is replaced with a new artificial hip joint. Total hip replacement surgery is an option to relieve severe arthritis pain that limits your daily activities.
Revision hip replacement is advised for the following conditions:
Revision hip replacement surgery is performed under general anaesthesia. During the procedure, your surgeon will make an incision over the hip to expose the joint. Then, the femur is dislocated from the acetabulum so that the old plastic liner and metal socket can be removed from the acetabulum.
After removal, the acetabulum is prepared using extra bone and wire mesh to make up for the socket space and shape. Then, the new metal shell is inserted into the socket using screws or special cement. A liner made of plastic, ceramic or metal is placed inside the metal socket.
To prepare the femoral component, the top of the femur bone is cut into several pieces to remove the implant. The segments of bone are cleaned and the new femoral implant is inserted into the femur either by a press fit or using bone cement. The segments of the femur and the femoral component are held together with surgical wires. Then the femoral head component made of metal or ceramic is placed on the femoral stem. All the new components are secured in place to form the new hip joint. The muscles and tendons around the new joint are repaired and the incision is closed.
After undergoing revision hip replacement, you must take special care to prevent the new joint from dislocating and to ensure proper healing. Some of the common precautions to be taken include:
As with any major surgical procedure, there are certain potential risks and complications involved with revision hip replacement surgery. The possible complications after revision hip replacement include:
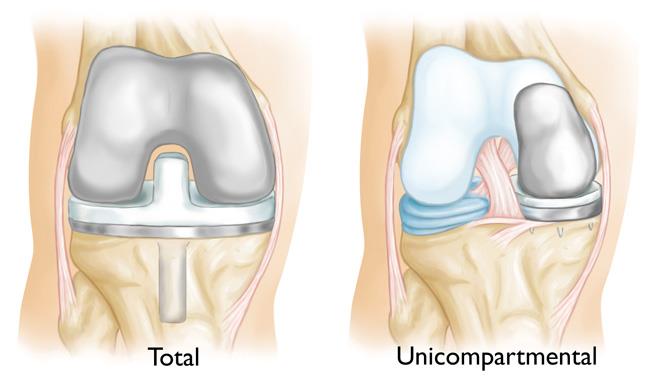
The knee is a complex hinge joint. A unicompartmental knee replacement becomes necessary once all medical treatments have been exhausted. The diseased knee joint is usually isolated to the medial side (inside) of the knee and it becomes so badly damaged that, in spite of painkillers, it causes significant pain which interferes with your quality of life. The purpose of surgery is to relieve pain and therefore improve function and quality of life.
Unicompartmental knee replacement is normally considered when the joint cartilage is worn down to bone on the medial side of the knee, with relative preservation of the rest of the joint. It can also be performed on the lateral (outside) side of the joint. It is becoming an increasingly popular procedure and long term results are excellent.
Surgery either takes place under a general anaesthetic or with an anaesthetic injection in the back (spinal anaesthetic) with or without sedation.
The operation usually takes between one and one and a half hours. It usually involves resurfacing the end of the femur (thigh bone) and top of the tibia (shin) on the medial side of the knee joint with a cemented metal femoral components and a plastic fixed tibial component. The patella (kneecap) is left alone.
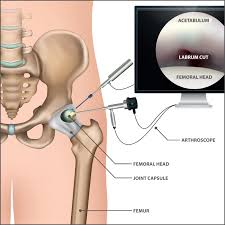
Hip arthroscopy, also referred to as keyhole or minimally invasive surgery, is a procedure in which an arthroscope is inserted into your hip joint to check for any damage and repair it simultaneously.
An arthroscope is a small, fibre-optic instrument consisting of a lens, light source, and video camera. The camera projects images of the inside of the joint onto a large monitor, allowing your surgeon to look for any damage, assess the type of injury and repair the problem.
Hip arthroscopy is a surgical procedure performed through very small incisions to diagnose and treat various hip conditions including:
Hip arthroscopy is performed under regional or general anaesthesia depending on you and your surgeon’s preference. Your surgeon will make 2 or 3 small incisions about 1/4 inch in length around the hip joint. Through one of the incisions an arthroscope is inserted. Along with it, a sterile solution is pumped into the joint to expand the joint area and create room for the surgeon to work.
The larger image on the television monitor allows your surgeon to visualise the joint directly and determine the extent of damage so that it can be surgically treated. Surgical instruments will be inserted through other tiny incisions to treat the problem. After the surgery, the incisions are closed and covered with a bandage.
The advantages of hip arthroscopy over the traditional open hip surgery include:
Your surgeon may advise you to take certain precautions to promote faster recovery and prevent further complications. These include:
As with any surgery, there are potential risks and complications involved. It is very important that you are informed of these risks before you decide to proceed with hip arthroscopy surgery. The possible risks and complications may include:

1. Poly trauma cases
2. Communited long bone fractures
3. Complex peri articular fractures
1. Screws
2. Plates
3. K wires
4. Nails
5. External fixators
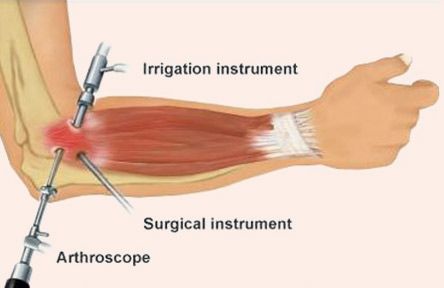
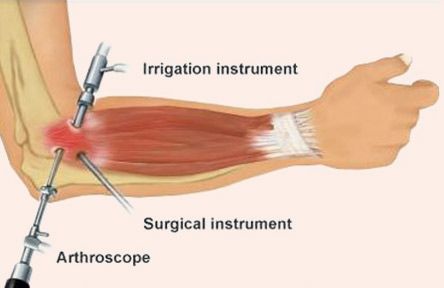
Arthroscopy is a minimally invasive procedure that allows your surgeon to look inside the elbow joint using small incisions (portals) and instruments. Elbow arthroscopy allows the surgeon to diagnose and treat the disorders of the elbow.
The elbow is the joint that connects the upper arm bone and the forearm bones. Elbow joint helps in movement of the arms forward, backward, as well as to twist the arms inside and outside. Elbow joint may get affected by inflammation, injury, or other disease conditions causing severe pain and requiring surgical treatment.
Conditions of the elbow that can be treated by arthroscopy include
Elbow arthroscopy is performed under local or general anaesthesia.
Your surgeon makes a few incisions near your elbow joint. Through one of the incision, an arthroscope, having a small camera fixed to the end of a narrow fiber-optic tube which is inserted. The camera magnifies and projects images of the elbow on a large screen monitor which helps in diagnosing the condition. Through the other incisions surgical instruments are inserted to treat the problem of the elbow. A sterile solution is injected into the elbow to expand the joint that allows clear view of the joint and provides extra room for the procedure. After the surgery the stitches are closed and dressing is applied.
You are most often discharged on the same day of your elbow arthroscopy. Your surgeon will place a splint that immobilizes that will prevent the movement of the elbow until it is healed completely. The operated elbow should be elevated to prevent excessive swelling and pain. A rehabilitation program may also be advised for a successful recovery. Therapeutic exercises aim to restore motion and strengthen the elbow.
After the surgery, Always remember to keep the operated area clean and dry to prevent infection and pus formation.
Recovery after the surgery depends on the type of procedure performed. Recovery from simple procedures is often fast. Recovery from elbow arthroscopy is much faster than that from an open wrist surgery.
Some of the advantages of arthroscopy are smaller incisions, minimal soft tissue trauma, less pain, faster recovery time, low infection rate, less scarring, earlier mobilization, and allows patient to go home the same day.
Elbow arthroscopy is a safe procedure; complications are very rare. Complications specific to elbow arthroscopy include bleeding in the elbow joint, infection, elbow stiffness, blood clots or continuing elbow problems.

Arthroscopy is a minimally invasive procedure that allows your surgeon to look inside the wrist joint using small incisions (portals) and instruments. Wrist arthroscopy allows the surgeon to diagnose and treat the disorders of the wrist.
Wrist is also called as carpus, a complex joint comprised of bones and joints, ligaments and tendons, nerves, blood vessels, and muscles that hold the bones together. A fibrous cartilage present between the radius and ulna (forearm bones of the hand) separates the radioulnar joint from the rest of the wrist. Wrist connects the forearm to the hand and allows it to move. Carpal tunnel is an opening in the wrist through which the nerves and blood vessels pass.
Some of the common problems of the wrist which can be treated by arthroscopy include
Wrist arthroscopy is performed under local or general anaesthesia.
Your surgeon makes a few incisions near your wrist joint. Through one of the incision, an arthroscope, having a small camera fixed to the end of a narrow fiber-optic tube which is inserted. The camera magnifies and projects images of the wrist on a large screen monitor which helps in diagnosing the condition. Through the other incisions surgical instruments are inserted to treat the problem of the wrist. A sterile solution is injected into the wrist to expand the joint that allows clear view of the joint and provides extra room for the procedure. After the surgery the stitches are closed and dressing is applied.
You are most often discharged on the same day of your wrist arthroscopy. Your surgeon will place a cast or a splint that immobilizes that will prevent the movement of the wrist until it is healed completely. The operated wrist should be elevated to prevent excessive swelling and pain. Ice (wrapped over a cloth) can be applied over the operated area which helps to reduce swelling and medications are taken to reduce pain. A rehabilitation program may also be advised for a successful recovery. Therapeutic exercises aim to restore motion and strengthen the wrist.
After the surgery, Always remember to keep the operated area clean and dry to prevent infection and pus formation.
Recovery after the surgery depends on the type of procedure performed. Recovery from simple procedures is often fast. Recovery from wrist arthroscopy is much faster than that from an open wrist surgery.
Some of the advantages of arthroscopy are smaller incisions, minimal soft tissue trauma, less pain, faster recovery time, low infection rate, less scarring, earlier mobilization, and allows patient to go home the same day.
Wrist arthroscopy is a safe procedure; complications are very rare. Complications specific to wrist arthroscopy include bleeding in the wrist joint, infection, wrist stiffness, blood clots or continuing wrist problems.
Arthroscopy is a minimally invasive procedure that allows your surgeon to look inside the ankle joint using small incisions (portals) and instruments. Ankle arthroscopy allows the surgeon to diagnose and treat the disorders of the ankle.
The ankle consists of three bones attached by muscles, tendons, and ligaments that connect the foot to the leg.
In the lower leg are two bones called the tibia (shin bone) and the fibula. These bones articulate (connect) to the Talus or ankle bone at the tibiotalar joint (ankle joint) allowing the foot to move up and down.
An Ankle Arthroscopy can be useful in patients who have a variety of painful ankle conditions. These include:
Ankle arthroscopy is performed under local or general anaesthesia.
Your surgeon makes a few incisions near your ankle joint. Through one of the incision, an arthroscope, having a small camera fixed to the end of a narrow fiber-optic tube which is inserted. The camera magnifies and projects images of the elbow on a large screen monitor which helps in diagnosing the condition. Through the other incisions surgical instruments are inserted to treat the problem of the elbow. A sterile solution is injected into the ankle to expand the joint that allows clear view of the joint and provides extra room for the procedure. After the surgery the stitches are closed and dressing is applied.
You are most often discharged on the same day of your ankle arthroscopy. Pain medicines are prescribed to manage pain. Crutches may be recommended for several weeks. A rehabilitation program may also be advised for a successful recovery. Therapeutic exercises aim to restore motion and strengthen the muscles of the leg and ankle.
Recovery after the surgery depends on the type of procedure performed. Recovery from simple procedures is often fast. Recovery from ankle arthroscopy is much faster than that from an open ankle surgery.
Some of the advantages of arthroscopy are smaller incisions, minimal soft tissue trauma, less pain, faster recovery time, low infection rate, less scarring, earlier mobilization, and allows patient to go home the same day./p>
Ankle arthroscopy is a safe procedure; complications are very rare. Complications specific to ankle arthroscopy include bleeding in the ankle joint, infection, ankle stiffness, blood clots or continuing ankle problems.
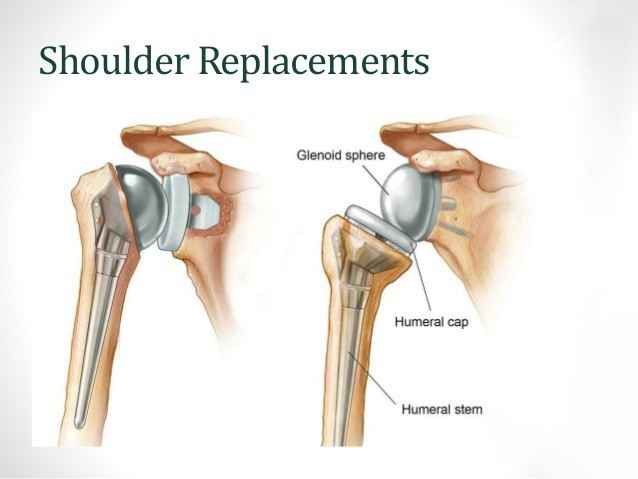
The shoulder is a highly movable body joint that allows various movements of the arm. It is a ball and socket joint, where the head of the humerus (upper arm bone) articulates with the socket of the scapula (shoulder blade) called the glenoid. The two articulating surfaces of the bones are covered with cartilage, which prevents friction between the moving bones. The cartilage is lubricated by synovial fluid. Tendons and ligaments around the shoulder joint provide strength and stability to the joint.
When the cartilage is damaged, the two bones rub against each other resulting in pain, swelling and stiffness of the joint (osteoarthritis).
Total shoulder replacement surgery is performed to relieve these symptoms. In this surgery, the damaged articulating parts of the shoulder joint are removed and replaced with artificial prostheses. Replacement of both the humeral head and the socket is called a total shoulder replacement.
Total shoulder joint replacement surgery is indicated for conditions such as osteoarthritis or rheumatoid arthritis when medication, injections, physical therapy, and activity changes do not help relieve pain. Your doctor recommends surgery when you have the following symptoms:
To decide whether total shoulder replacement is a good option for you the surgeon will evaluate your condition thoroughly.
Your surgeon reviews your medical history and performs a physical examination of your shoulder to assess the extent of mobility and pain. Imaging tests such as X-ray or MRI (magnetic resonance imaging) are ordered.
The surgery is done under regional or general anesthesia. An incision is made over the affected shoulder and the underlying muscles are separated to expose the shoulder joint. The surgery may be performed as open surgery, where a large incision is made, or minimally invasive, where small incisions are made to insert an arthroscope (a thin tube with a camera and light source) and surgical tools.
The upper arm bone (humerus) is separated from the glenoid socket of the shoulder bone. The arthritic or damaged humeral head is cut and the humerus bone is hollowed out and filled with cement. A metal ball with a stem, is gently press fit into the humerus.
Next, the arthritic part of the socket is prepared. The plastic glenoid component is fixed in the shoulder bone.
After the artificial components are implanted, the joint capsule is stitched and the wound is closed.
After the surgery, pain medications and antibiotics are prescribed to control pain and prevent infection. Your arm may be secured in a sling or cast. The rehabilitation program includes physical therapy, which is started soon after the surgery and is very important to strengthen and provide mobility to the shoulder. You may be able to perform gentle daily activities two to six weeks after surgery.
As with any major surgery, there may be potential risks involved: